|
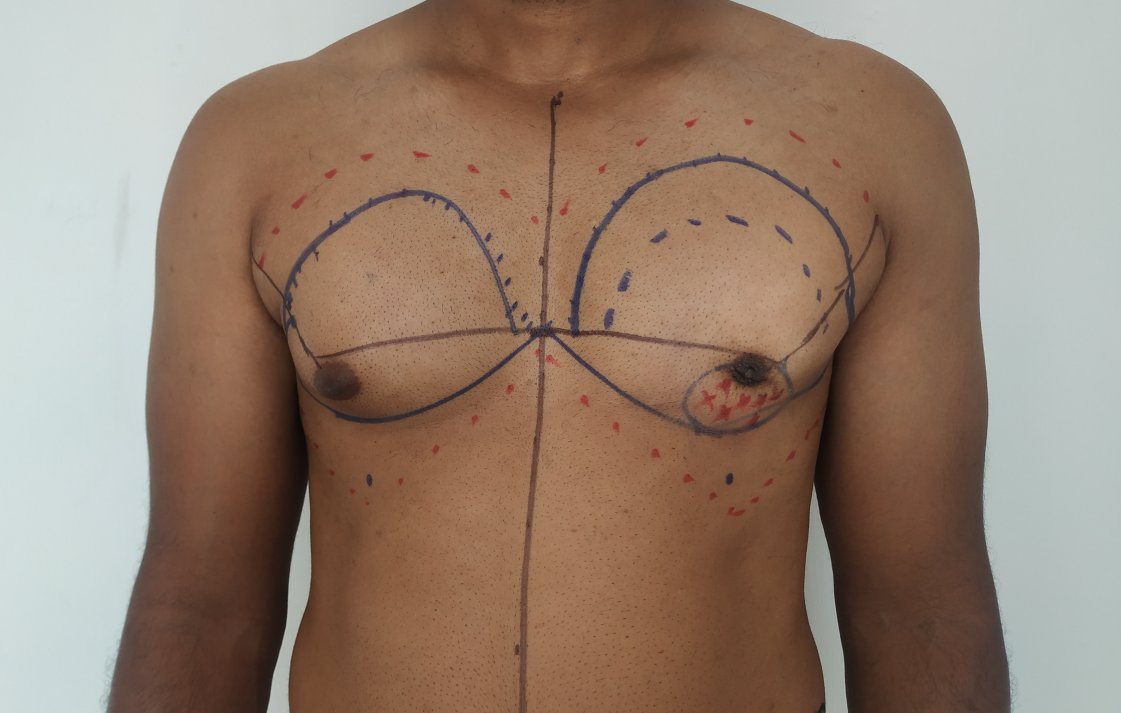
Gynecomastia, or enlarged male breasts, is a common condition that we treat in our medical practice. Many patients express concerns about potential complications from gynecomastia surgery. However, it's important to note that gynecomastia surgery is generally a safe procedure, and complications are uncommon. The risk of complications can be further lowered by addressing modifiable risk factors. This video discusses the various aspects that can help patients avoid complications from gynecomastia surgery. Some key points covered in the video include: - Proper patient selection and evaluation - Surgical techniques to minimize tissue trauma - Strategies to manage postoperative swelling and bleeding - Importance of following postoperative care instructions By understanding these factors, patients can feel more confident about the safety and outcomes of gynecomastia surgery. The video provides a comprehensive overview to help address common concerns and ensure the best possible results for our patients.
0 Comments
1. Why do gynecomastia surgery?
Gynecomastia correction is done to improve the appearance. This helps in reducing the sense of shame and discomfort with the appearance. 2. What are the steps for undergoing gynecomastia correction?
3. What is the cost of the procedure? Would there be additional costs? The cost of the procedure depends on the anesthesia (local vs general), and the deformity (extent of liposuction and need for skin resection). In most patients, the surgical cost of liposuction and gland excision comes to approximately 70,000 rupees. The additional costs include stay and investigations. These may cost you an additional 5000 rupees. 4. Are there any EMI schemes? We do not offer any loan or EMI scheme. We do not encourage individuals to take loans for procedures. In case of any financial difficulties, you could talk to one of us. 5. Which anesthesia is used for correction? Most of our procedures are done under local anesthesia. General anesthesia is usually done for anxious individuals or those who require skin resection (removal). Modern anesthesia protocols are safe. 6. Which surgical procedure is carried out for gynecomastia correction? The steps depend on the deformity. In most of our patients we do the following:
7. What is the recovery following gynecomastia correction? Most patients have an uneventful recovery. We recommend the following:
8. I stay far away. Can I come directly for surgery? We do not encourage combining consultation and procedure at one visit. We believe an individual needs additional time to understand the procedure, possible outcomes, and complications. We also require investigation reports to rule out any other issues. Hence we advise a separate visit for the consultation before the procedure. 9.Can I come to the surgery alone? No. We want you to be accompanied by a close relative or a dependable friend. This is for the following reasons,
10. I'm staying abroad. I want to get it done during my vacation. Are there any additional steps that I should take? We advise the following to such individuals:
11. Are there any risks to life? Modern anaesthesia protocols are very safe. So any serious complications are very unlikely. 12. Will I get a recurrence? Most patients do not get a recurrence. Individuals who are prone to recurrence are those below 18 years of age and secondary gynecomastia. For more information please click here. 1.എന്തുകൊണ്ടാണ് ഗൈനക്കോമാസ്റ്റിയ ശസ്ത്രക്രിയ നടത്തുന്നത്? കാഴ്ച മെച്ചപ്പെടുത്താൻ ഗൈനക്കോമാസ്റ്റിയ ശസ്ത്രക്രിയ നടത്തുന്നു. ഇത് കാഴ്ചയിൽ നാണക്കേടും അസ്വസ്ഥതയും കുറയ്ക്കാൻ സഹായിക്കുന്നു. 2. ഗൈനക്കോമാസ്റ്റിയ ശസ്ത്രക്രിയയ്ക്ക് വിധേയമാക്കുന്നതിനുള്ള ഘട്ടങ്ങൾ എന്തൊക്കെയാണ്? 1. കൺസൾട്ടേഷൻ: ഞങ്ങൾ നിങ്ങളെ പരിശോധിക്കുന്നു. ക്ലിനിക്കൽ കണ്ടെത്തലുകളെ അടിസ്ഥാനമാക്കി ഒരു ചികിത്സാ പദ്ധതി ഞങ്ങൾ നിർദ്ദേശിക്കുന്നു. 2. ലാബ് പരിശോധനകൾ. അവയിൽ ഹോർമോണുകളുടെ അളവ് സംബന്ധിച്ച പരിശോധനകൾ ഉൾപ്പെടുന്നു.ശസ്ത്രക്രിയയ്ക്കുള്ള ഫിറ്റ്നസ് വിലയിരുത്തുന്നതിന് മറ്റ് പരിശോധനകൾ നടത്തുന്നു. നിങ്ങളുടെ വീടിനടുത്തുള്ള ലാബിൽ ഇവ ചെയ്യാവുന്നതാണ്. 3. നടപടിക്രമം: ശസ്ത്രക്രിയയെത്തുടർന്ന് ആശുപത്രിയിൽ രാത്രി താമസമുണ്ട്. മറ്റൊരു ജില്ലയിലേക്ക് യാത്ര ചെയ്യേണ്ടി വരുന്ന രോഗികൾ ഒരു ദിവസം കൂടി താമസിക്കണം. 4. തുടർ സന്ദർശനങ്ങൾ: ശസ്ത്രക്രിയയുടെ അടുത്ത ദിവസം ഡ്രെയിനുകൾ നീക്കം ചെയ്യുകയും ഡ്രെസ്സിംഗുകൾ മാറ്റുകയും ചെയ്യും. നിങ്ങൾ വീട്ടിലെത്തിക്കഴിഞ്ഞാൽ ആദ്യത്തെ ഫോളോ അപ്പ് 2 ആഴ്ചയ്ക്ക് ശേഷമാണ്. പിന്നീടുള്ള സന്ദർശനങ്ങൾ 1 മാസം, 3 മാസം, 6 മാസങ്ങളിലാണ്. 3. ശസ്ത്രക്രിയയുടെ ചെലവ് എത്രയാണ്? അധിക ചിലവുകൾ ഉണ്ടാകുമോ? ശസ്ത്രക്രിയയുടെ ചെലവ് അനസ്തേഷ്യ (ലോക്കൽ vs ജനറൽ), വൈകല്യം (ലിപ്പോസക്ഷൻ്റെ വ്യാപ്തിയും ത്വക്ക് വിഭജനത്തിൻ്റെ ആവശ്യകതയും) എന്നിവയെ ആശ്രയിച്ചിരിക്കുന്നു. മിക്ക രോഗികളിലും ലിപ്പോസക്ഷൻ്റെയും ഗ്ലാൻ എക്സിഷൻ്റെയും ശസ്ത്രക്രിയാ ചെലവ് ഏകദേശം 70,000 രൂപ വരും. അധിക ചെലവുകളിൽ താമസവും ലാബ് അന്വേഷണവും ഉൾപ്പെടുന്നു. ഇവയ്ക്ക് നിങ്ങൾക്ക് 5000 രൂപ അധികമായി ചിലവായേക്കാം. 4. എന്തെങ്കിലും EMI സ്കീമുകൾ ഉണ്ടോ? ഞങ്ങൾ ഒരു ലോണും EMI സ്കീമും വാഗ്ദാനം ചെയ്യുന്നില്ല. നടപടിക്രമങ്ങൾക്കായി വായ്പ എടുക്കുന്നതിൽ നിന്ന് ഞങ്ങൾ വ്യക്തികളെ പ്രോത്സാഹിപ്പിക്കുന്നില്ല. എന്തെങ്കിലും സാമ്പത്തിക ബുദ്ധിമുട്ടുകൾ ഉണ്ടെങ്കിൽ ഞങ്ങളിൽ ഒരാളോട് സംസാരിക്കാം. 5. ശസ്ത്രക്രിയയ്ക്ക് ഏത് അനസ്തേഷ്യയാണ് ഉപയോഗിക്കുന്നത്? ഞങ്ങളുടെ മിക്ക നടപടിക്രമങ്ങളും ലോക്കൽ അനസ്തേഷ്യയിലാണ് ചെയ്യുന്നത്. ഉത്കണ്ഠയുള്ള വ്യക്തികൾക്കോ ചർമ്മം നീക്കം ചെയ്യേണ്ടവർക്കോ സാധാരണയായി ജനറൽ അനസ്തേഷ്യ ചെയ്യാറുണ്ട്. ആധുനിക അനസ്തേഷ്യ പ്രോട്ടോക്കോളുകൾ സുരക്ഷിതമാണ്. 6. ഗൈനക്കോമാസ്റ്റിയയ്ക്ക് ഏത് തരത്തിലുള്ള ശസ്ത്രക്രിയയാണ് നടത്തുന്നത്? ഞങ്ങളുടെ മിക്ക രോഗികളിലും ഞങ്ങൾ ഇനിപ്പറയുന്നവ ചെയ്യുന്നു: 1.ലിപ്പോസക്ഷൻ. കൊഴുപ്പ് നീക്കം ചെയ്യുന്നതിനാണ് ഇത് ചെയ്യുന്നത്. ഇത് മികച്ച രൂപം ലഭിക്കാനും നടപടിക്രമം സുരക്ഷിതമാക്കാനും സഹായിക്കുന്നു. 2.ഗ്രന്ഥി നീക്കം ചെയ്യൽ. ഏരിയോളയിൽ (മുലക്കണ്ണിന് ചുറ്റുമുള്ള ചർമ്മം) ഒരു ചെറിയ മുറിവിൻ്റെ സഹായത്തോടെയാണ് ഇത് ചെയ്യുന്നത്. ഞങ്ങളുടെ മിക്ക രോഗികളിലും ഞങ്ങൾ ചർമ്മം നീക്കം ചെയ്യുന്നില്ല. 7. ഗൈനക്കോമാസ്റ്റിയ ശസ്ത്രക്രിയയ്ക്ക് ശേഷം എനിക്ക് എപ്പോഴാണ് ജോലിയിലേക്ക് മടങ്ങാൻ കഴിയുക? ഇനിപ്പറയുന്നവ ഞങ്ങൾ ശുപാർശ ചെയ്യുന്നു:
8. ഞാൻ ദൂരെയാണ് താമസിക്കുന്നത്. എനിക്ക് ശസ്ത്രക്രിയയ്ക്ക് നേരിട്ട് വരാമോ? ഒരു സന്ദർശനത്തിൽ കൺസൾട്ടേഷനും ശസ്ത്രക്രിയയും സംയോജിപ്പിക്കുന്നത് ഞങ്ങൾ പ്രോത്സാഹിപ്പിക്കുന്നില്ല. ശസ്ത്രക്രിയ, ഫലങ്ങൾ, സങ്കീർണതകൾ എന്നിവ മനസ്സിലാക്കാൻ ഒരു വ്യക്തിക്ക് കൂടുതൽ സമയം ആവശ്യമാണെന്ന് ഞങ്ങൾ വിശ്വസിക്കുന്നു. മറ്റേതെങ്കിലും പ്രശ്നങ്ങൾ ഒഴിവാക്കുന്നതിന് ഞങ്ങൾക്ക് ലബോറട്ടറി അന്വേഷണ റിപ്പോർട്ടുകളും ആവശ്യമാണ്. അതിനാൽ, നടപടിക്രമത്തിന് മുമ്പ് കൂടിയാലോചനയ്ക്കായി ഒരു പ്രത്യേക സന്ദർശനം ഞങ്ങൾ നിർദ്ദേശിക്കുന്നു. 9. എനിക്ക് ഒറ്റയ്ക്ക് സർജറിക്ക് വരാമോ? ഇല്ല. നിങ്ങളോടൊപ്പം ഒരു അടുത്ത ബന്ധുവോ സുഹൃത്തോ ഉണ്ടായിരിക്കണമെന്ന് ഞങ്ങൾ ആവശ്യപ്പെടുന്നു. ഇത് ഇനിപ്പറയുന്ന കാരണങ്ങളാലാണ്, ചില വ്യക്തികൾക്ക് ശസ്ത്രക്രിയാനന്തര കാലഘട്ടത്തിൽ സഹായം ആവശ്യമായി വന്നേക്കാം. നടപടിക്രമത്തെക്കുറിച്ചും ചികിത്സാ പദ്ധതിയിലെ എന്തെങ്കിലും മാറ്റങ്ങളെക്കുറിച്ചും ഒരു വ്യക്തി ബോധവാനായിരിക്കണമെന്ന് ഞങ്ങൾ ആവശ്യപ്പെടുന്നു. ഒരാൾ കൂടെയുണ്ടെങ്കിൽ അത് മാനസികാരോഗ്യത്തിന് സഹായിക്കുന്നു. 10. ഞാൻ വിദേശത്താണ് താമസം. എൻ്റെ അവധിക്കാലത്ത് അത് പൂർത്തിയാക്കാൻ ഞാൻ ആഗ്രഹിക്കുന്നു. ഞാൻ എന്തെങ്കിലും അധിക നടപടികൾ സ്വീകരിക്കേണ്ടതുണ്ടോ? അത്തരം വ്യക്തികൾക്ക് ഞങ്ങൾ ഇനിപ്പറയുന്നവ ഉപദേശിക്കുന്നു:
11. ജീവന് എന്തെങ്കിലും അപകടങ്ങൾ ഉണ്ടോ? ആധുനിക അനസ്തേഷ്യ പ്രോട്ടോക്കോളുകൾ വളരെ സുരക്ഷിതമാണ്. അതിനാൽ, ഗുരുതരമായ സങ്കീർണതകൾ ഉണ്ടാകാനുള്ള സാധ്യത വളരെ കുറവാണ്. 12. എനിക്ക് ഗൈനക്കോമാസ്റ്റിയ വീണ്ടും വരുമോ? മിക്ക രോഗികൾക്കും ഗൈനക്കോമാസ്റ്റിയയുടെ ആവർത്തനം ലഭിക്കുന്നില്ല. 18 വയസ്സിന് താഴെയുള്ളവരും ദ്വിതീയ ഗൈനക്കോമാസ്റ്റിയയുമാണ് ആവർത്തനത്തിന് സാധ്യതയുള്ള വ്യക്തികൾ. കൂടുതൽ വിവരങ്ങൾക്ക് ദയവായി ഇവിടെ സന്ദർശിക്കുക In our practice we frequently come across concerns about the pain associated with gynecomastia surgery both during and after the procedure. Thoughts about the pain can lead to a lot of anxiety in those affected by this condition. It may even prevent some individuals from seeking treatment.
Pain is subjective. Pain is a protective sensation that helps animals avoid injury. Postoperative pain is due to the stimulation of the nerve endings at the operated site. The use of pain medications help reduce the discomfort. Modifications in the surgical technique can contribute to less pain. Gynecomastia surgery is a short stay procedure. Patients can go home without a prolonged inpatient stay. This is made possible due to adequate pain relief with oral medicines. There are a few reasons for less pain following a gynecomastia correction whn compared to other surgical procedures. These include,
Most patients do not require more than oral medications for postoperative comfort. This is more so among individuals treated under local anaesthesia. Local anaesthesia helps identify nerve sparing and address it before the completion of the procedure. Nerve sparing my occur when the procedure is performed under general anesthesia. Fear about pain can discourage many from getting surgery. But the improvements in anaesthesia and newer surgical technique, lead to a comfortable postoperative period in most individuals. They usually do not require more than a few oral pain medicines in the initial few days following surgery. To learn more about gynecomastia, click here. Liposuction is a part of the treatment of gynecomastia correction in most of our patients. It is relatively uncommon to do a gynecomastia correction without accompanying liposuction. Why so?
Liposuction has many advantages. They include the following:
There are instances when we may not do liposuction during gynecomastia surgery. But these are relatively uncommon. Liposuction is sometimes not done in thin individuals with less breast fat. Such individuals usually present with a gland enlargement confined to the area under the areola. They also have a very thin skin pinch. In such situations, we proceed with a gland excision through an areolar incision after local anesthetic infiltration. Liposuction has many benefits when done in gynecomastia treatment. It is usually done in almost all cases of gynecomastia surgery in our practice. To learn more about gynecomastia, please click here. Gynecomastia is excess breast tissue in men. In a subset of individuals with gynecomastia, there can be redundant or excess skin. The excess skin affects the outcomes following a gynecomastia corrective surgery. It can mean a longer duration to achieve an acceptable outcome. In some cases, we may do additional surgery to take care of excess skin.
How does skin redundancy present in gynecomastia? Redundant skin is usually apparent with a clinical examination. The breast tissue tends to sag in such individuals. The breasts appear deflated. There can be visible folds on the lower part, and lateral areas of the chest. The presence of ptosis or sagging gives an aged appearance to the chest. Who are the individuals prone to get skin redundancy associated with gynecomastia? The risk factors associated with excess skin in gynecomastia include:
What are the treatment strategies that can be adopted in case of skin excess? hereAmong individuals with excess body weight, it is always recommended to lose weight before undergoing a surgical correction. Optimizing the body weight before surgery has certain advantages. It is easier to assess the extent of excess skin before surgery. This makes the surgical outcome more predictable. In some cases, we may opt to undertake skin reduction during the time of gynecomastia correction. With weight loss, patients can benefit from the skin recoil beforehand. In an individual, with excess skin, gynecomastia correction can be done in two different ways. It can be done either with skin excision or without skin excess. Both strategies lead to different outcomes. When the correction is carried out without a skin excision there may be a postoperative course with an increase in the deflated appearance. This usually improves with time due to the skin recoil. It may take many months before the full extent of skin recoil is appreciated. We usually advise our patients to wait as much as 8 months before deciding on an additional surgery to remove the skin excess. Many patients are usually satisfied with the skin recoil and choose not to have any skin excision procedures. This has the advantage of an initial simpler procedure with shorter scars. Skin excisional procedures are associated with longer and more visible scars. The second strategy would include gynecomastia correction carried out with simultaneous skin excision. The pattern of the excision can vary depending on the extent of skin excess. Patients with more excess tend to have a greater amount of skin removed. With this technique, the excess skin is addressed in a single procedure. However, it carries the disadvantage of longer scars. In our practice, this approach is less commonly used. We tend to choose individuals with severe excess for this approach. What are the steps that can be taken by an individual to address excess skin? The excess skin is usually seen to accompany increased body weight. Individuals should try to maintain their weight close to ideal. This is usually achieved with the help of dietary modifications such as diet and exercise. Weight training helps recruit the excess skin and contributes to reduced sagging over the lower part of the chest. Weight training and accompanying muscle hypertrophy also bring along aesthetic benefits. Excess skin is seen in some individuals presenting with gynecomastia. This is more commonly seen in those with excess body weight. The skin excess can be tackled with surgery in a staged or simultaneous way. Both strategies have their advantages and disadvantages. A treatment plan is chosen based on individual preferences and extent of excess skin. Individuals with skin excess can help improve this condition with appropriate dietary modifications and exercise. Learn more about gynecomastia here. Secondary corrections refer to operations undertaken to improve the outcome after primary surgery. Secondary corrections for gynecomastia are done to improve the appearance of the operated site.
Some of the deformities that may be corrected with secondary surgery include the following:
Timing of secondary corrections of gynecomastia. We usually wait for a year before undertaking secondary corrections. This has some advantages. They include the following,
Various procedures are undertaken during secondary gynecomastia corrections. These may be carried out in isolation or as a combination. They include,
A surgical plan is based on the appearance of the deformity and concerns of the patient. In other words, such plans are customized. Two patients with a similar-looking deformity may undergo different types of surgical correction. A realistic expectation is important since it is usually only possible to make some improvements in the appearance. Also, secondary corrections are usually taken after a year following the primary surgery. During this period patients can help optimize their appearance by the following activities.
Secondary corrections of gynecomastia can help improve the appearance of selected individuals. For more information about gynecomastia please visit: https://www.amicusclinic.in/gynecomastia I could also have gone for a title called ‘why am I fond of syringe liposuction?’. Liposuction is a technique in cosmetic surgery for removing fat cells from certain parts of the body. The fat cells amenable to liposuction are between the skin and muscles. We do not perform liposuction on fat deeper than the muscles. Liposuction may be part of another procedure like abdominoplasty or gynecomastia correction.
Liposuction involves the creation of a vacuum. This vacuum helps remove fat cells with small cannulas. Such cannulas are called liposuction cannulas. Cannulas vary depending on their diameter, length, and shape of openings near the end. We use different types of cannulas based on the area treated. During liposuction, a vacuum is obtained by a machine or a syringe. Syringe liposuction employs a syringe for generating liposuction. A cannula is attached to one end of the syringe. After insertion of the cannula inside the body, the surgeon pulls back the piston and locks it in place. The vacuum created inside the syringe helps move the fat cells into the syringe during to and fro movement. Once the syringe gets filled, the cannula is disconnected and the fat is emptied. The same process gets repeated till the desired endpoint is reached. This constitutes syringe liposuction. Syringe liposuction is a simple technique with a lot of benefits. This makes it popular among many practitioners. Some of the benefits include the following,
Syringe liposuction was introduced by Toledo in 1989. The advantages of this technique make it very endearing to some practitioners of liposuction. One of them includes me. For more information about liposuction, please click here. For more information about gynecomastia, please click here. Do I have gynecomastia?
'I don't know if I have gynecomastia. Maybe it is fat. So, I came.' I hear this often in my practice. Gynecomastia is male breast enlargement. It can be diagnosed easily because of its appearance. But sometimes, the presentation can be a bit confusing. The breast tissue is seen under the nipple and areola. The areola is the pigmented skin immediately surrounding the nipple. Depending on the severity of enlargement, gynecomastia can present as puffiness of the nipple and areola, or it can extend towards the sides of the chest. It can affect one side or both sides. Both sides can look different. In other words, there can be asymmetry. The word, ‘gynecomastia’ comes from ‘gyneco’ and 'mastia'. 'Gyneco' means female, and ‘mastia’ means breast. Thus gynecomastia translates into the female-looking breast. This occurs due to an enlargement of the breast tissue. Compared to female breasts, male breasts are positioned more laterally (meaning to the side of the chest). Hence, the deformity of gynecomastia is also especially pronounced when viewed from the side. Hypertrophy of the underlying muscle (pectoralis major) looks different from that of the breast. The muscle animates (moves) in certain maneuvers. This means the muscle contracts during certain activities like flexing the arm against resistance. Also, the lower border of the muscle usually stops at the level of the nipple. Any enlargement that significantly extends below the level of the areola is usually due to breast tissue. The lower border of the muscle is straight or flat. This is easily made out in men who perform weight training. The presence of breast tissue tends to make the inferior border curved. The curved lower part of the breast gives it a feminine appearance. It is also possible to pinch the breast tissue separately from the underlying tissues. We usually carry this out during a clinical examination of an individual presenting with gynecomastia. Puffiness of the nipple and areola is also associated with enlargement of the breast tissue. It is not associated with hypertrophy of the underlying muscle. There is an entity called pseudogynecomastia. ‘Pseudo’ means false. This is due to increased fat deposits in the chest. There is no glandular enlargement in pseudogynecomastia. It is usually seen in the setting of obesity with fat deposits that mimic the appearance of male breast enlargement. Losing weight will lead to an improvement in the deformity associated with pseudogynecomastia. It is usually simple to diagnose a case of gynecomastia during a clinical examination. We sometimes request additional investigations to look for any underlying cause for gynecomastia. Imaging can help us to confirm the condition. Most cases of gynecomastia are benign and are self-limiting. Surgery is undertaken when gynecomastia results in significant distress in the affected individual. To learn more about gynecomastia, please visit, https://www.amicusclinic.in/gynecomastia Beauty is associated with proportions. A body part that is disproportionate to the rest of the body can impair appearance. An example would be women with arms that are large when compared to the torso. It is a common aesthetic concern in plastic surgery practice.
Arms are tubular structures. They consist of soft tissues around a bone. The soft tissues are made up of structures like fat, muscles, and vessels. It is surrounded by skin. Large arms usually involve a relative excess of fat and skin. The fat occupies the layer deeper to the skin. As the volume of fat increases, the overlying skin stretches to adjust to the increased volume. Hence, a reduction in the size of the arms involves a reduction in the size of the fat and skin excess. We can achieve this through surgical, and non-surgical techniques. Why do some individuals get big arms? The increase in the size of the arms is associated with excess weight. This excess fat gets deposited in various areas of the body. Some of us tend to deposit this fat more in our arms. This intrinsic tendency varies from one individual to another. Other conditions can be associated with an increased size of the arms, lymphedema, soft tissue swellings, etc. But they are relatively less common causes of big arms. This article deals with the management of the arms as a result of excess fatty tissue. What can be done to improve the appearance? A reduction in the size of arms has to address the two types of tissues involved, namely fatty tissue and skin. First, the fat. Fat occupies the area between the muscles and skin. The amount of fatty tissue correlates with the amount that can be rolled between two fingers. Fat is amenable to dietary modifications. A reduction in body weight usually leads to a reduction in the amount of fatty tissue and a resulting in a decrease in the size of arms. Liposuction is a surgical technique to remove the fatty tissue with the help of small tubes (cannula). It is useful for individuals with fatty tissue that is resistant to dietary modifications. A good candidate for liposuction is someone with close to ideal body weight. Liposuction does not directly address the excess skin. Next, the skin. The skin stretches to accommodate the excess fatty tissue. Once there is a reduction in the fatty tissue with diet or liposuction, there is a recoil of this skin. Recoil is the shrinking of the skin to a smaller area. However, this recoil of the skin takes time. It can take as much as a year for the skin to maximally recoil. In cases of massive weight loss, the recoil can be incomplete. This is seen as a persistent loose fold(s) of the skin. It is usually seen on the undersurface of the arms. Skin recoil is also reduced with advancing age and in smoking. Brachioplasty is a surgical procedure to remove excess skin. During brachioplasty, skin is removed as an ellipse from the medial surface (inside) of the arm. This is the part of the skin that abuts the torso. The decision to undertake a brachioplasty is taken after waiting for the skin to maximally recoil. Hence, it is usually not carried out during liposuction. The extent of skin removal is customized depending upon the extent of skin excess. Brachioplasty helps in improving the contour by removing the loose skin folds. What are the advantages of the management of this condition? It helps in improving the appearance of the arms in individuals with disproportionately large arms. The role of diet and exercise play a very important role in the appearance of the arms. Liposuction and brachioplasty are two surgical procedures that help to further optimize the appearance of arms. Gynecomastia is an enlargement of the male breast. It is a common condition. Surgical correction of gynecomastia achieves a reduction in the excess breast tissue. A reduction in the breast tissue helps improve the aesthetics of the male chest. In most cases, surgery involves liposuction and gland excision. Liposuction addresses fat, and direct removal addresses the gland. These two steps are usually adequate for most individuals with gynecomastia. However, this may be insufficient to restore the aesthetics in those with excess skin. They may require additional treatments.
The stretched-out skin usually recoils adequately after reduction in most of the individual. The problem relating to excess skin is observed commonly in two subsets of patients. They are,
How do we manage excess skin while treating gynecomastia? The treatment approach depends on the presentation. We tend to follow a conservative wait and watch in younger individuals, and those with a less severe presentation. This is because of better skin recoil in younger individuals. Also, the removal of the gland will reduce the effect of the weight on the skin. This helps the skin to recoil better. It is common practice to wait for more than ten months to assess the full extent of skin recoil. Any secondary corrections are done after this period. The conservative approach may not help in older individuals and those with severe forms of excess. In such cases, we may opt to add a skin removal procedure during the management of gynecomastia. Good candidates for primary correction of the skin would include nonsmokers. They must have a stable weight. Skin removal procedures in those with unstable weight may result in suboptimal outcomes. The design of the skin excess is variable. This is based on the extent of skin excess and patient preferences. A circumareolar (around the areola) approach is preferred in milder cases. In individuals with severe excess, we prefer extensile (long) incisions with the grafting of the nipple and areola. Needless to say, individuals with longer incisions have longer scars. What is the advantage of staging a skin removal procedure? In other words, why wait between a gynecomastia correction and a skin excisional procedure. Skin can recoil significantly with time. It may not be able to predict the full extent. Adequately recoiled skin results in acceptable aesthetics. The full extent of skin recoil after gynecomastia correction takes time. Avoiding a skin removal procedure means lesser scars. However, this approach may not be suitable in those with severe forms of skin excess. Are there any approaches to prevent this issue with excess skin? They would include the following. Avoiding excess body weight. The excess skin problem is not common in individuals with normal or ideal body weight. Early treatment of gynecomastia. The ability of the skin to recoil reduces with age. Smoking is bad for skin recoil. Nonsmokers tend to have better outcomes when compared to smokers. What is the advantage of managing the excess skin in individuals with gynecomastia? It leads to better aesthetic outcomes. For more information about gynecomastia please visit here. |
AuthorI like to keep it simple. CategoriesArchives
June 2024
Categories |
- Home
-
Cosmetic
- Fat grafting
- Swellings and moles
- Scar revision
- Leukoderma (Melanocyte transfer)
- Hair transplant
- Facial rejuvenation procedures
- Nose job (Rhinoplasty)
- Cleft lip nose correction
- Ear (Otoplasty)
- Lip reduction
- Breast augmentation
- Breast reduction
- Tuberous breasts
- Axillary breasts
- Gynecomastia
- Liposuction
- Brachioplasty (Arm contouring)
- Abdominoplasty (Tummy tuck)
- Female genital rejuvenation
-
Reconstructive
- Contact
- Blog
- Home
-
Cosmetic
- Fat grafting
- Swellings and moles
- Scar revision
- Leukoderma (Melanocyte transfer)
- Hair transplant
- Facial rejuvenation procedures
- Nose job (Rhinoplasty)
- Cleft lip nose correction
- Ear (Otoplasty)
- Lip reduction
- Breast augmentation
- Breast reduction
- Tuberous breasts
- Axillary breasts
- Gynecomastia
- Liposuction
- Brachioplasty (Arm contouring)
- Abdominoplasty (Tummy tuck)
- Female genital rejuvenation
-
Reconstructive
- Contact
- Blog
You can leave us a comment using the contact form below.
We shall get back to you at the earliest.
We shall get back to you at the earliest.
Links
- Face procedures | Rhinoplasty, Otoplasty, Lip reduction, Fat grafting
- Body procedures | Gynecomastia , Breast reduction, Abdominoplasty, Brachioplasty, Liposuction
- Skin procedures | Scar revision, Moles, Leukoderma surgery
Let's be friends !
Follow us at Facebook and Twitter.
Follow us at Facebook and Twitter.
© 2024 Amicus Clinic (Plastic Surgery Centre, Trivandrum). All rights reserved.






 RSS Feed
RSS Feed



